 Unlike physicians and human health-care practitioners, veterinarians cannot prescribe cannabis for medical purposes for their animal patients. Under the Cannabis Act, cannabis for medical purposes applies to humans only. Unlike physicians and human health-care practitioners, veterinarians cannot prescribe cannabis for medical purposes for their animal patients. Under the Cannabis Act, cannabis for medical purposes applies to humans only.
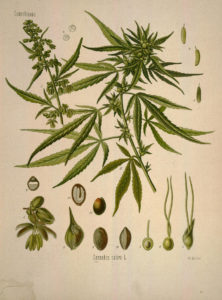
Under the Cannabis Act, prescription drugs derived from cannabis are a legal pathway for access to cannabis for animals. All phytocannabinoids, including CBD and all the other naturally occurring active ingredients in cannabis plants, have been placed on the Prescription Drug List and, therefore, they are subject to the Food and Drugs Act and Regulations as well. There are currently no approved cannabis-derived prescription drugs for animals, meaning there is no legal pathway for veterinarians to obtain or dispense these products for animals in Canada. CBD products currently being marketed and sold in Canada for use in pets are operating outside of the current legislative framework.
Legally purchased recreational cannabis from authorized provincial retail sales outlets can be distinguished from black market cannabis by its packaging. Legal products:
- Are packaged and labeled according to strict rules set by Health Canada;
- Have packaging with a CRA excise stamp on it;
- Do not make health claims;
- Do not have an indication for animal use; and
- Undergo quality control to ensure, among other things, that concentrations of CBD and THC that are indicated on the label are accurate, and free of specified contaminants (e.g. certain pesticides, mold toxins, heavy metals)
Veterinarians may advise clients on the use of legally available recreational cannabis for their pets based on sound professional judgment.
At this time there are no Health Canada approved cannabis products for veterinary use. For this reason, veterinarians are unable to prescribe or recommend cannabis products for our patients.
However, if this is a product you are already using, or you would like to add it to your pet’s medical plan, I may guide you on the safe use of legally available recreational cannabis products.
As part of your consultation, we will discuss the treatment goals you have and the benefits (and drawbacks) of adding cannabis to your pet’s medical therapy plan.
How comfortable are you with purchasing an extract product or plant material to extract yourself, administering the product, and monitoring your pet for its effects?
The consultation also consists of a complete review of medical records including current diet, medications, supplements and any other therapies in use, potential drug-drug and drug-herb interactions, and analysis of products being used. Follow up visits will fine-tune therapies until the treatment goals have been met.

https://www.cavcm.com/resources-for-pet-families
Most of us know about the importance of Vitamin D in maintaining not only healthy bones, but in the function of the immune system and preventing cancer. Most physicians recommend that people in the northern half of North America take between 1000 and 3000 IU daily over the winter months when there is not enough exposure to sun for our bodies to produce this essential vitamin. What about our pets?
Unfortunately our companion animals do not even produce Vitamin D from sunshine in the hottest sunniest summer months as their skin lacks the enzyme to convert sunshine to the vitamin that we all need. Almost 100% of their vitamin D must be taken in from the food.
A recent study showed that a majority of dogs are lacking this essential vitamin. This was true for dogs on commercial diets as well as on home prepared diets . But some dogs eating the same food had low levels and other had adequate levels. What does this tell us? There is no way to know if your pet has enough Vitamin D without doing a blood test. Once the test is done we can tell if the level is in the optimal range, or if a supplement needs to be given. Disorders of the bowel and kidney can lead to low levels so it is especially important for dogs and cats with those illnesses to have their levels tested. A simple blood test can give us the answer, and the sample can be drawn at the same time as other early-detection and wellness blood screening tests.
Over the past few months I have been routinely running the Vitamin D level test, and the results to date show that an overwhelming number of my patients are deficient in Vitamin D and require a supplement.
For more information, see the research article
It breaks our hearts to see a loved one in pain. Too often we miss the signs in companion dogs and cats because they are very subtle. If pain is acute, like when a puppy plays too roughly at the park, he squeals, and we know that he is hurt. But adult dogs can be very stoic and not vocalize at all, even when in extreme pain. Chronic pain is even more challenging because the animal has learned to expect it and is dealing with it at all times. Cats especially do not show symptoms that are easily recognizable. Cats that display any weakness such as pain are at risk of becoming another predator’s meal; they instinctively mask pain. The signs of pain are so very subtle that it is easy to miss them unless you are extremely observant and spend a lot of time with the cat. Often they stop doing the things that are difficult for them like jumping up on the counter or playing with their toys. We often assume they are “just getting old” because their activity level declines, and the changes are gradual. We used to miss a lot of pain in veterinary medicine practice, but we are getting much better now at identifying and treating it.
For more on how pain affects behaviour and how to figure out if your pet is in pain, see
http://www.veterinarypartner.com/Content.plx?P=A&S=0&C=0&A=1761
http://www.catvets.com/cat-owners/caring-for-cats/signs-and-symptoms
What I really want to talk about is how to treat pain safely and naturally with herbs, and let you know which can be safely combined with narcotics, non-steroidal anti-inflammatories (NSAIDS) or both.
First of all I need to get something off my chest. One of my pet peeves is the issue of over-the-counter supplement quality and safety. Many products have no third-party evaluation for purity and potency, and even have inaccurate or missing label information on the exact source and processing of the herb. In my practice I only use professional-grade products from companies I trust, who share manufacturing details such as GMP and ISO certification, and use DNA or chemical “fingerprinting” to ensure that the plant material is the correct species and potency. Most are members in good standing of industry associations such as NASC .
These products are more expensive than some out there in the online stores and local pet shops. You usually get what you pay for.
Now, on to what you are really here for….
Turmeric, Curcuma longa (root), which contains curcumin, is one of my favourite herbs for pain releif, but it has very LOW bioavailability as a raw herb powder. It acts on nitric oxide pathways instead of the COX pathways that NSAIDS block, so it is safe to combine with those drugs. Use the raw powder mixed with fat in a home-cooked meal or “gravy” for your pet to increase absorption or choose a cucurmin product that is complexed with lecithin or choline so your pet can benefit.
In Traditional Chinese Medicine, the different parts of the root are used differently. The Rhizome, Jiang Huang is used more for pain, especially in the forelimbs, while the Tuber, Yu Jin is used more for liver disorders.
Alfalfa, Medicago sativa (above-ground parts: leaf, stem and flower) is a nourishing and restoring herb. It is usually used as a componant in herbal formulas for pain, not often on its own. Constituents include phytoestrogens, Calcium, vitamins A, C, E, and K, saponin, and phenols.
Corydalis, Corydalis ambigua (root) called Yan Hu Suo in chinese is an excellent analgesic, especially for cancer pain. It inhibits dopamine release in the brain, so caution should be used if combining with medications that change dopamine levels. It lowers blood pressure and interacts with calcium channel blocker heart medications. As well, it can inhibit platelets which potentially leads to increased risk of bleeding, of special concern if surgery is planned.
Many more herbs are used for pain, and will be explored in future posts.
Before using any supplement for your pet, please consult with a qualified veterinary herbalist.
To find a qualified veterinary herbalist near you, check VBMA’s practitioner list.
I recently had a question about what can cause shaking, especially in the legs of an older dog. The most common cause of shaking legs in the young dog that I see is fear- these are dogs that do not want to be in the examination room! But for the older dog shaking at home, muscle weakness is often the root cause. Several systemic illnesses can result in muscle weakness. Kidney disease often causes loss of muscle tissue as well as imbalances in the electrolytes, various minerals that are essential for muscle function. Adrenal gland disease can also cause muscle loss and electrolyte imbalances. Cancer must always be on the list as well, due to the unpredictable nature of the disease. Systemic disorders are diagnosed with blood and urine testing, sometimes x-rays and ultrasound as well, usually on an outpatient basis. Therapy can include dietary modifications, mineral supplementation and physical therapy, as well as medications where needed.
Pain from arthritis is an often unrecognized factor in shaky legs and muscle weakness. When it is more difficult to get up and move, your pet exercises less, and muscles gradually atrophy. While leg joints such as hips, knees and elbows are often affected, don’t forget all the joints in the back. As many of us know, when the back hurts, everything hurts.
Acupuncture and cold-laser therapy are the basic tools that I utilize for my patiens with arthritis. Prolotherapy and stem cell therapy very successful, but are more “invasive” interventions, and must be done with sedation or anesthesia, so are not suitable for all pets. Massage is wonderful because it is usually available from travelling therapists who will come to your home. Some massage techniques are also very easy to learn to do yourself, and are a special close bonding experience for you and your dog or cat. Herbal and nutritional interventions such as high levels of omega-3’s from fish oil, green-lipped muscle extract, cucurmin (turmeric extract), MSM, glucosamine etc. can be very effective in reducing the pain and mobility restrictions of arthritis. Physical therapy is also a very valuable part of a multi-modal approach to arthritis, to help strengthen muscles and the tissues that support the joints.
For more on integrative arthritis care, please read “Arthritis Therapy: Integrative Approach”
There is great upcoming opportunity available, but only to the first 12 people to respond!
Hilary Watson, veterinary nutritionist, and Janet Craig, a licensed chef, are offering Canine Culinary 101, a workshop to train owners how to prepare home-cooked dog food recipes safely and in bulk using a community kitchen.
Normally these classes cost $55 per person; you receive 4 kilograms of food at the end of class.
A private class is being planned for Dr. Sherebrin and her clients, at a special reduced ratre of $10 per person.
Date: TBA, Bloor-Sherbourne area
A 3-hour cooking workshop AND 4 kilos of healthy prepared dog food for only $10.00!
What owners should bring:
• Tupperware storage containers or large
Ziploc bags that can hold 4 kg of food
• an apron
• a small cutting board
• a knife of choice
• a jar of HILARY’S BLEND supplement*
If you need to purchase a jar of Hilary’s Blend supplement, please let me know ASAP to allow time to order in stock.
No experience necessary! Novices very welcome!
Enjoy the company of other dog owners who
are as committed to their dog’s health as you are!
Pass this message along to any others who may be interested.
contact: info@mytcmvet.com
Differences between Holistic, Integrative, Naturopathic, Alternative and Homeopathic therapies and practices:
Do you use holistic, homeopathic and naturopathic interchangeably? Have you ever discussed holistic health and discovered that the other person was defining holistic totally differently? This is not surprising, since no accepted standards exist for holistic, holistic health, or holistic medicine.
Many people, myself included, define holistic as a whole made up of interdependent parts; an inclusive view of the animal in its environment, encompassing its relationships with other pets and the guardian (family). When applied to illness, it is called holistic medicine and includes a number of factors, such as dealing with the root cause of an illness; increasing client involvement; and considering both conventional (allopathic) and complementary (alternative) therapies.
Some people use Holistic as a synonym for alternative therapies. By this definition, “going holistic” means turning away from all conventional medical options and using alternative treatment exclusively. This meaning mainly relates to illness situations, and sometimes is used for controversial therapies.
Integrative Medicine is the combiantion of conventional and alternative therapies, using multiple modalities to gain the “best of both worlds”.
Naturopathic Medicine is focused on prevention and the use of natural treatment options to promote healing.
Alternative Medicine is defined as modalities of therapy that have not been taught or embraced by colleges of veterinary medicine, used in place of conventional therapies. This definition is very fluid, as different universities in different locations in the world all have variations in what is taught. Over time this also changes. For example, 30 years ago, essential fatty acid supplements were alternative, now they are mainstream. Alternative therapies can include a wide range of modalities such as: acupuncture, chinese and western herbs, orthomolecular medicine, nutritional supplements, low-level laser therapy, Tellington Touch, acupressure, Reiki, Craniosacral therapy, chiropractic, flower essences, ozone therapy, homeopathy, massage and many other modalities.
Complementary Medicine is defined as modalities that are not taught or embraced by colleges of veterinary medicine, used in addition to conventional therapies (see Integrative Medicine)
Homeopathy from the Greek words homoios (similar) and pathos (suffering) is an entire system of medicine, notable for its practice of prescribing water-based solutions that contain extremely diluted ingredients. The theory of homeopathy was developed by the Saxon physician Samuel Hahnemann (1755–1843) and first published in 1796. Homeopathy calls for treating “like with like” (law of similars). The practitioner considers the totality of symptoms of a given case. He or she then chooses a homeopathic remedy that has been reported in a homeopathic proving to produce a similar set of symptoms in healthy subjects. This remedy is usually given in extremely low concentrations.
It seems like all you hear about these days is prebiotics and probiotics. Television advertisements, food and drink packaging, supplements, all proclaiming that they are extra special because they contain prebiotics or probiotics or both. Continue reading Prebiotics, Probiotics, Antibiotics: What’s Bugging You?
|
|
 Unlike physicians and human health-care practitioners, veterinarians cannot prescribe cannabis for medical purposes for their animal patients. Under the Cannabis Act, cannabis for medical purposes applies to humans only.
Unlike physicians and human health-care practitioners, veterinarians cannot prescribe cannabis for medical purposes for their animal patients. Under the Cannabis Act, cannabis for medical purposes applies to humans only.













