Please send me questions or topics that you want an integrative or tcvm approach to….Dr.Sherebrin at mytcmvet.com
|
Under the Cannabis Act, prescription drugs derived from cannabis are a legal pathway for access to cannabis for animals. All phytocannabinoids, including CBD and all the other naturally occurring active ingredients in cannabis plants, have been placed on the Prescription Drug List and, therefore, they are subject to the Food and Drugs Act and Regulations as well. There are currently no approved cannabis-derived prescription drugs for animals, meaning there is no legal pathway for veterinarians to obtain or dispense these products for animals in Canada. CBD products currently being marketed and sold in Canada for use in pets are operating outside of the current legislative framework. Legally purchased recreational cannabis from authorized provincial retail sales outlets can be distinguished from black market cannabis by its packaging. Legal products:
Veterinarians may advise clients on the use of legally available recreational cannabis for their pets based on sound professional judgment. At this time there are no Health Canada approved cannabis products for veterinary use. For this reason, veterinarians are unable to prescribe or recommend cannabis products for our patients. However, if this is a product you are already using, or you would like to add it to your pet’s medical plan, I may guide you on the safe use of legally available recreational cannabis products. As part of your consultation, we will discuss the treatment goals you have and the benefits (and drawbacks) of adding cannabis to your pet’s medical therapy plan. How comfortable are you with purchasing an extract product or plant material to extract yourself, administering the product, and monitoring your pet for its effects? The consultation also consists of a complete review of medical records including current diet, medications, supplements and any other therapies in use, potential drug-drug and drug-herb interactions, and analysis of products being used. Follow up visits will fine-tune therapies until the treatment goals have been met.
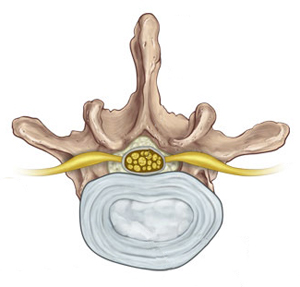
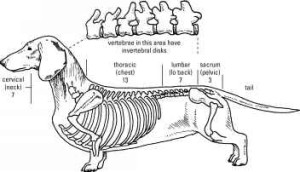
Join your colleagues October 22-23, 2016 in downtown Toronto for the Annual General Meeting of the Association of Veterinary Acupuncturists of Canada. Dr. Neal Sivula, DVN, PhD, FAAVA will be lecturing on acupuncture from a neurological perspective for internal medicine, musculoskeletal and neurological disorders. Acupuncture case presentations and Round Table discussions to share different approaches to common issues. Early bird discounts- REGISTER NOW for best price! EXTENDED EARLY REGISTRATION DEADLINE NOW AUG.22 Fall weekend registration form October 2016 Fall weekend CE Neal Sivula brochure Fall weekend CE call for cases We are offering registration discounts to our colleagues who present a case for the Round Table discussion. There is still space for a few cases, but case presentations are on a first-come first served basis so don’t delay. Most of us know about the importance of Vitamin D in maintaining not only healthy bones, but in the function of the immune system and preventing cancer. Most physicians recommend that people in the northern half of North America take between 1000 and 3000 IU daily over the winter months when there is not enough exposure to sun for our bodies to produce this essential vitamin. What about our pets? Over the past few months I have been routinely running the Vitamin D level test, and the results to date show that an overwhelming number of my patients are deficient in Vitamin D and require a supplement. For more information, see the research article The effect of diet on serum 25-hydroxyvitamin D concentrations in dogsFor many people, the cutest dog breeds are the small ones; dacshunds, poodles, bichons, shi-tzus and others typically referred to as toy breeds. Unfortunately these breeds are also over-represented in the caseload of patients with intervertebral disc disease, also referred to by its initials IVDD. It is sometimes called a “slipped disc” or “herniated disc”. It is caused by degeneration of one or more of the shock-absorbing pillow-shaped discs located between the vertebral bones of the spine. These discs can become hardened and stiff (calcium deposits form inside them) causing bulging of the disc into the spinal canal, or they may rupture, letting the soft jelly-like material they contain out into the canal. There is really only enough room for the spinal cord in the spinal canal, so it gets compressed and sometimes irreparably damaged. When the spinal cord or the nerves passing out of it to the body are compressed, pain and impairment of neural function are the result. Some dogs show minimal symptoms but stop doing things that hurt such as going up or down stairs, jumping on the bed or going about their usual activities. An observant guardian may sometimes notice a change in gait, a wobble or hitch in their step, especially when turning or changing directions. Others may have severe and unrelenting pain and refuse to move, eat or void their bowels or bladder. in the most severe cases there is no pain- all sensation and movement beyond the location of the spinal cord damage is lost, resulting in complete paralysis. Damage to the spinal cord causes a loss of communication between the brain and the body. Most dogs that have grade 2-4 IVDD will remain permanently impaired, if they are able to regain their ability to walk at all. There are 27 discs (or more in some long-backed breeds such as dachsunds, basset hounds and corgis) between the vertebral bones from the nape of the neck to the tail. Since the disease in a degeneration, multiple discs may be affected. A recent veterinary study at The Royal Veterinary College in the United Kingdom established a relationship between long backs, short legs and IVDD. Early treatment is critical for IVDD. In cases of unrelenting pain or paralysis, an MRI of the spinal cord to determine location of damage followed immediately by surgery to remove the herniated disc material is usually recommended. Unfortunately this surgery only has a success rate of 50%. Intensive acupuncture with electrostimulation and physical rehabilitation is essential for return to full function, or as full as posible depending on the extent of spinal cord damage. For back pain only with no loss of nerve function (such as loss of spatial sensation, called proprioceptive deficits) the treatments are started at twice a week and taper quickly to once a month for maintenance. For paralysis the treatments will be daily to every third day until sensation returns. Nursing care for these dogs is critical, as bladder and bowel function is lost as well. Poor hygeine can lead to bedsores, bladder infections and painful skin rashes. So if you have a long-bodied, short-legged dog in your family, be aware of this devastating disease and keep an eye out for the little signs you might otherwise miss. Regular acupuncture treatments can not only help keep your dog’s back flexible and healthy but the veterinary acupuncturist will check for subtle signs at every visit to catch and treat dysfunction before pain and disability occur. It breaks our hearts to see a loved one in pain. Too often we miss the signs in companion dogs and cats because they are very subtle. If pain is acute, like when a puppy plays too roughly at the park, he squeals, and we know that he is hurt. But adult dogs can be very stoic and not vocalize at all, even when in extreme pain. Chronic pain is even more challenging because the animal has learned to expect it and is dealing with it at all times. Cats especially do not show symptoms that are easily recognizable. Cats that display any weakness such as pain are at risk of becoming another predator’s meal; they instinctively mask pain. The signs of pain are so very subtle that it is easy to miss them unless you are extremely observant and spend a lot of time with the cat. Often they stop doing the things that are difficult for them like jumping up on the counter or playing with their toys. We often assume they are “just getting old” because their activity level declines, and the changes are gradual. We used to miss a lot of pain in veterinary medicine practice, but we are getting much better now at identifying and treating it. For more on how pain affects behaviour and how to figure out if your pet is in pain, see http://www.veterinarypartner.com/Content.plx?P=A&S=0&C=0&A=1761 http://www.catvets.com/cat-owners/caring-for-cats/signs-and-symptoms
What I really want to talk about is how to treat pain safely and naturally with herbs, and let you know which can be safely combined with narcotics, non-steroidal anti-inflammatories (NSAIDS) or both. First of all I need to get something off my chest. One of my pet peeves is the issue of over-the-counter supplement quality and safety. Many products have no third-party evaluation for purity and potency, and even have inaccurate or missing label information on the exact source and processing of the herb. In my practice I only use professional-grade products from companies I trust, who share manufacturing details such as GMP and ISO certification, and use DNA or chemical “fingerprinting” to ensure that the plant material is the correct species and potency. Most are members in good standing of industry associations such as NASC . These products are more expensive than some out there in the online stores and local pet shops. You usually get what you pay for. Now, on to what you are really here for…. Turmeric, Curcuma longa (root), which contains curcumin, is one of my favourite herbs for pain releif, but it has very LOW bioavailability as a raw herb powder. It acts on nitric oxide pathways instead of the COX pathways that NSAIDS block, so it is safe to combine with those drugs. Use the raw powder mixed with fat in a home-cooked meal or “gravy” for your pet to increase absorption or choose a cucurmin product that is complexed with lecithin or choline so your pet can benefit. In Traditional Chinese Medicine, the different parts of the root are used differently. The Rhizome, Jiang Huang is used more for pain, especially in the forelimbs, while the Tuber, Yu Jin is used more for liver disorders. Alfalfa, Medicago sativa (above-ground parts: leaf, stem and flower) is a nourishing and restoring herb. It is usually used as a componant in herbal formulas for pain, not often on its own. Constituents include phytoestrogens, Calcium, vitamins A, C, E, and K, saponin, and phenols. Corydalis, Corydalis ambigua (root) called Yan Hu Suo in chinese is an excellent analgesic, especially for cancer pain. It inhibits dopamine release in the brain, so caution should be used if combining with medications that change dopamine levels. It lowers blood pressure and interacts with calcium channel blocker heart medications. As well, it can inhibit platelets which potentially leads to increased risk of bleeding, of special concern if surgery is planned. Many more herbs are used for pain, and will be explored in future posts. Before using any supplement for your pet, please consult with a qualified veterinary herbalist. To find a qualified veterinary herbalist near you, check VBMA’s practitioner list.
 A chair is not a good enough barrier
Powered by Twitter Tools
Powered by Twitter Tools
Powered by Twitter Tools
Powered by Twitter Tools |
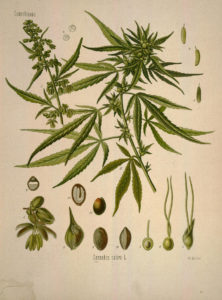 Unlike physicians and human health-care practitioners, veterinarians cannot prescribe cannabis for medical purposes for their animal patients. Under the Cannabis Act, cannabis for medical purposes applies to humans only.
Unlike physicians and human health-care practitioners, veterinarians cannot prescribe cannabis for medical purposes for their animal patients. Under the Cannabis Act, cannabis for medical purposes applies to humans only.